…. a revolution in mental health care
Attention Deficit Hyperactivity Disorder
Attention Deficit Hyperactivity Disorder (ADHD)
Dr. Mabel Lopez is a Neuropsychologist with extensive experience in the diagnosis and treatment of Attention Deficit Hyperactivity Disorder (ADHD). She has provided education to both patients and providers on this topic. She has trained other psychologists in the area regarding the neurocognitve circuits involved in ADHD.
Because of the complexity of ADHD, Dr. Lopez will NOT diagnose ADHD with a checklist. Rather, she will conduct a structured clinical interview, thorough neuropsychological evaluation, and gather relevant collateral to determine the veracity of ADHD and need for further intervention. She works closely with medical doctors in the area in the event medication management were warranted.
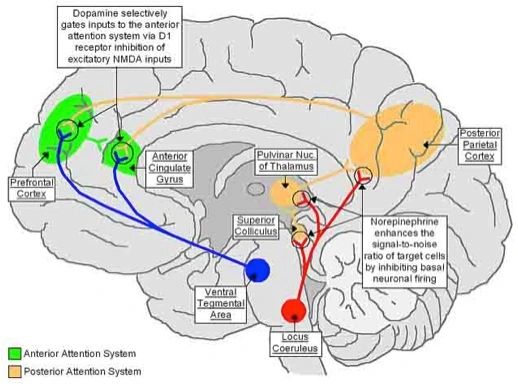
Neuropsychology plays a key role in the diagnosis of ADHD because Neurocognitive Deficits are a hallmak feature of ADHD. ADHD is a distinct brain disorder. The attention system is complex and spans from the pre-frontal cortex (dopaminergic system) to posterior parietal region (norepinergic system) to the cerebellum (see Figure above).
Disruption can occur to any part of this system, explaining why ADHD is such a heterogeneous condition. Moreover, in addition to problems in the attention domain (concentration, selective attention, divided attention, cognitive set shifting, inhibition, working memory and processing speed), the neuropsychological evaluation can provide insights into other aspects of cognition that may be affected in ADHD such as intelligence, learning, memory, visuospatial skills, language, reasoning.
Finally, individuals with ADHD often have co-occurring problems with specific learning disability. Formal academic functioning can be assessed to tease out aptitude from ability.
The American Psychiatric Association's Diagnostic and Statistical Manual, Fifth edition (DSM-5), includes changes for the diagnosis of ADHD:
- symptoms can now occur by age 12 rather than by age 6
- several symptoms now need to be present in more than one setting rather than just some impairment in more than one setting
- new descriptions were added to show what symptoms might look like at older ages
- for adults and adolescents age 17 or older, only 5 symptoms are needed instead of the 6 needed for younger children.
DSM-5 Criteria for ADHD
People with ADHD show a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development:
1. Inattention: Six or more symptoms of inattention for children up to age 16, or five or more for adolescents 17 and older and adults; symptoms of inattention have been present for at least 6 months, and they are inappropriate for developmental level:
- Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
- Often has trouble holding attention on tasks or play activities.
- Often does not seem to listen when spoken to directly.
- Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., loses focus, side-tracked).
- Often has trouble organizing tasks and activities.
- Often avoids, dislikes, or is reluctant to do tasks that require mental effort over a long period of time (such as schoolwork or homework).
- Often loses things necessary for tasks and activities (e.g. school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
- Is often easily distracted
- Is often forgetful in daily activities.
2. Hyperactivity and Impulsivity: Six or more symptoms of hyperactivity-impulsivity for children up to age 16, or five or more for adolescents 17 and older and adults; symptoms of hyperactivity-impulsivity have been present for at least 6 months to an extent that is disruptive and inappropriate for the person’s developmental level:
- Often fidgets with or taps hands or feet, or squirms in seat.
- Often leaves seat in situations when remaining seated is expected.
- Often runs about or climbs in situations where it is not appropriate (adolescents or adults may be limited to feeling restless).
- Often unable to play or take part in leisure activities quietly.
- Is often "on the go" acting as if "driven by a motor".
- Often talks excessively.
- Often blurts out an answer before a question has been completed.
- Often has trouble waiting his/her turn.
- Often interrupts or intrudes on others (e.g., butts into conversations or games)
These criteria correspond to three distinct ADHD subtypes: inattentive, hyperactive, and combined type.
- Combined Presentation: if enough symptoms of both criteria inattention and hyperactivity-impulsivity were present for the past 6 months
- Predominantly Inattentive Presentation: if enough symptoms of inattention, but not hyperactivity-impulsivity, were present for the past six months
- Predominantly Hyperactive-Impulsive Presentation: if enough symptoms of hyperactivity-impulsivity but not inattention were present for the past six months.
Because symptoms can change over time, the presentation may change over time as well.
Because so many possible combinations of these criteria exist, ADHD is a very heterogeneous disorder.
To make matters even more complex, ADHD often co-occurs with many symptoms and or discreet disorders.
- Mood disorder: sadness, irritability, somatic expressions of mood (appetite, sleep)
- Anxiety: excessive worrying, phobias, history of trauma
- Social intelligence: ability to get along with others (peer group, siblings, younger and older children), understanding of societal norms, odd eccentric behavior, autism spectrum symptoms or disorder
- Oppositional Defiant Disorder: not obeying authority (parents, teachers),
- Conduct Disorder: “acting out behaviors,” destruction of property, aggression towards others, arson, hurting animals, stealing, using or selling illicit substances, truant behaviors, problems with the law
- Learning Disability: learning problems at school, list subjects that are particularly troublesome. Note: most people with attention deficits have difficulty learning in general. It is important to determine whether learning difficulties due to attention deficits versus frank dyslexia, dyscalculia, or dysgraphia.
- Substance Abuse: abusing prescription medications (stimulants are addictive!), illicit drugs, or alcohol. This can occur at any age but adolescence period is at greater risk for onset in person’s with ADHD.
- Low self-esteem: feeling poorly, unworthy because of problems paying attention, learning, etc
- Pervasive Developmental Delays: intellectual disability, delays in language or motor functioning
- Sleep Disorder: this is particularly important in ADHD because sleep disorder mimic ADHD symptoms. Symptoms to keep in mind are snoring, difficulty falling or staying asleep, broken sleep, light sleep, deep sleep, narcolepsy & cataplexy, early morning rising, daytime sleepiness, day-night confusion. Access for sleep aids, night time sleep routines, structure/enforcement of sleep schedule at home.
ADHD Assessment
Do you, or someone you love, experience a persistent pattern of inattention and/or hyperactivity-impulsivity that disrupts everyday functioning? Maybe ADHD is the reason, let Mind and Brain Care evaluate that possibility.